Most of us are aware of his life — the vision that changed how we see the digital world today. Through a series of revolutionary products and innovations that reshaped entire industries and society itself, it won’t be an overstatement to say that Apple has now become royalty in the field of technology and its advancement.
The man behind that innovation is Steve Jobs, who started Apple in the garage of his parents' home in 1976. In fact, while the company was founded in the garage, the initial work on the first computer, the Apple I, was completed in Jobs' own bedroom before moving to the garage.
Apple grew quickly enough to move out of the garage, and the rest is history.
Video
Although the world is well-versed with the story of Apple’s ascent and Jobs’ vision behind it, very few know how Jobs succumbed to death.
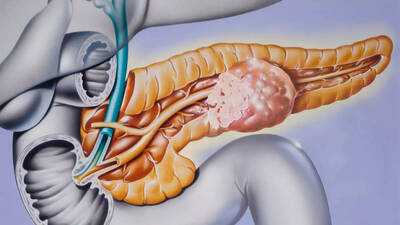
On October 5, 2011, Jobs died at just 56 from complications of pancreatic cancer. But the form of cancer that claimed his life wasn’t the aggressive “regular” type most people refer to when they hear “pancreatic cancer.” Jobs was diagnosed with a rare neuroendocrine tumor of the pancreas — a different beast entirely.
Jobs’ diagnosis: What happened
In October 2003, Steve Jobs was diagnosed with a tumor of the islet cells of the pancreas — a type known as a pancreatic neuroendocrine tumor (pNET), or islet-cell neuroendocrine tumor. He publicly announced the condition in mid-2004 and later underwent surgery to remove the tumor (a procedure called the Whipple operation or pancreaticoduodenectomy).
Initially, he chose to delay conventional treatment for about nine months, opting for alternative therapies (diet, acupuncture, herbal treatment) before finally consenting to surgery in July 2004.
In 2009, when the disease had progressed to the liver, Jobs underwent a liver transplant. His health continued to deteriorate, and he ultimately died from respiratory arrest caused by complications of his tumor.
It’s noteworthy that the form of pancreatic tumor he had is much less common and far less aggressive than the standard pancreatic adenocarcinoma.

What is a pancreatic neuroendocrine tumor and how it differs from “regular” pancreatic cancer
The most common type of pancreatic cancer (about 95% of cases) is pancreatic adenocarcinoma, which arises from the exocrine part of the pancreas (the part that produces digestive enzymes) — whereas Jobs’ tumor was an endocrine tumor of the islet cells (which make hormones), a pNET.
What are the key differences?
When it comes to growth rate and prognosis, pNETs tend to grow more slowly and have better survival rates when caught early. On the other hand, adenocarcinoma is aggressive, often diagnosed late, and has a very poor prognosis. Besides, adenocarcinoma is notoriously silent until advanced. Meanwhile, pNETs may manifest differently and — on the brighter side — sometimes are found much earlier.
Also See: Pancreas health: 5 symptoms that can help detect pancreatic cancer and pancreatitis early
Early signs and risk factors
One major challenge with all pancreatic cancers is that early symptoms are often quite vague and non-specific — think upper abdominal pain, weight loss, loss of appetite, jaundice (yellowing of skin and/or eyes) if the bile ducts are blocked. In the case of neuroendocrine tumors, they may sometimes produce hormone-related symptoms (depending on what hormone the tumor secretes), which come to attention comparatively sooner and hence can be found relatively quickly. Early detection remains difficult, so paying attention to persistent, unexplained symptoms and seeking medical evaluation promptly is the safest approach.
As for risk factors, they differ by the type of pancreatic cancer. While for the regular (adenocarcinoma) type, the known risk factors include smoking, obesity, chronic pancreatitis (perhaps alcohol-related), and family history, for neuroendocrine tumors of the pancreas, the risk factors are much less well-defined. For starters, heredity may play a role in some cases (e.g., in conditions such as Multiple Endocrine Neoplasia type 1 / MEN1), but many instances of pNET occur without obvious risk factors as well.
Mortality and survival rates
Pancreatic adenocarcinoma, by far, is one of the worst prognoses among cancers. Only around 10-15% are diagnosed when surgery is possible, and the five-year survival is often below 5–6%. For pNETs like Jobs had, the survival outlook is considerably better when it is detected early and receives proper treatment — in fact, surgical removal is more frequently successful if done at an early stage. In Jobs’s case, after his 2003 diagnosis (publicly announced in 2004), he lived until 2011 — he himself survived about eight years, which was longer than typical for pancreatic cancers. However, even for pNETs, once metastasis (such as to the liver) occurs, the disease becomes much harder to treat.
Video
The man behind that innovation is Steve Jobs, who started Apple in the garage of his parents' home in 1976. In fact, while the company was founded in the garage, the initial work on the first computer, the Apple I, was completed in Jobs' own bedroom before moving to the garage.
Apple grew quickly enough to move out of the garage, and the rest is history.
Video
Although the world is well-versed with the story of Apple’s ascent and Jobs’ vision behind it, very few know how Jobs succumbed to death.
On October 5, 2011, Jobs died at just 56 from complications of pancreatic cancer. But the form of cancer that claimed his life wasn’t the aggressive “regular” type most people refer to when they hear “pancreatic cancer.” Jobs was diagnosed with a rare neuroendocrine tumor of the pancreas — a different beast entirely.
Jobs’ diagnosis: What happened
In October 2003, Steve Jobs was diagnosed with a tumor of the islet cells of the pancreas — a type known as a pancreatic neuroendocrine tumor (pNET), or islet-cell neuroendocrine tumor. He publicly announced the condition in mid-2004 and later underwent surgery to remove the tumor (a procedure called the Whipple operation or pancreaticoduodenectomy).
Initially, he chose to delay conventional treatment for about nine months, opting for alternative therapies (diet, acupuncture, herbal treatment) before finally consenting to surgery in July 2004.
In 2009, when the disease had progressed to the liver, Jobs underwent a liver transplant. His health continued to deteriorate, and he ultimately died from respiratory arrest caused by complications of his tumor.
It’s noteworthy that the form of pancreatic tumor he had is much less common and far less aggressive than the standard pancreatic adenocarcinoma.

What is a pancreatic neuroendocrine tumor and how it differs from “regular” pancreatic cancer
The most common type of pancreatic cancer (about 95% of cases) is pancreatic adenocarcinoma, which arises from the exocrine part of the pancreas (the part that produces digestive enzymes) — whereas Jobs’ tumor was an endocrine tumor of the islet cells (which make hormones), a pNET.
What are the key differences?
When it comes to growth rate and prognosis, pNETs tend to grow more slowly and have better survival rates when caught early. On the other hand, adenocarcinoma is aggressive, often diagnosed late, and has a very poor prognosis. Besides, adenocarcinoma is notoriously silent until advanced. Meanwhile, pNETs may manifest differently and — on the brighter side — sometimes are found much earlier.
Also See: Pancreas health: 5 symptoms that can help detect pancreatic cancer and pancreatitis early
Early signs and risk factors
One major challenge with all pancreatic cancers is that early symptoms are often quite vague and non-specific — think upper abdominal pain, weight loss, loss of appetite, jaundice (yellowing of skin and/or eyes) if the bile ducts are blocked. In the case of neuroendocrine tumors, they may sometimes produce hormone-related symptoms (depending on what hormone the tumor secretes), which come to attention comparatively sooner and hence can be found relatively quickly. Early detection remains difficult, so paying attention to persistent, unexplained symptoms and seeking medical evaluation promptly is the safest approach.
As for risk factors, they differ by the type of pancreatic cancer. While for the regular (adenocarcinoma) type, the known risk factors include smoking, obesity, chronic pancreatitis (perhaps alcohol-related), and family history, for neuroendocrine tumors of the pancreas, the risk factors are much less well-defined. For starters, heredity may play a role in some cases (e.g., in conditions such as Multiple Endocrine Neoplasia type 1 / MEN1), but many instances of pNET occur without obvious risk factors as well.
Mortality and survival rates
Pancreatic adenocarcinoma, by far, is one of the worst prognoses among cancers. Only around 10-15% are diagnosed when surgery is possible, and the five-year survival is often below 5–6%. For pNETs like Jobs had, the survival outlook is considerably better when it is detected early and receives proper treatment — in fact, surgical removal is more frequently successful if done at an early stage. In Jobs’s case, after his 2003 diagnosis (publicly announced in 2004), he lived until 2011 — he himself survived about eight years, which was longer than typical for pancreatic cancers. However, even for pNETs, once metastasis (such as to the liver) occurs, the disease becomes much harder to treat.
Video
You may also like

Red swastikas drawn on Jewish buildings after NYC polls; mayor-elect Mamdani calls it 'disgusting act of antisemitism'

Lily Allen's open marriage woes confirm what I've known for a long time

Arsenal summer signing explains secret clean sheet tactic as Sunderland admission made

Keir Starmer's just been given another reason to worry - and he's 3,000 miles away

Meghan Markle's tea making parody video by TikTok star goes viral






